Keeping Warm And Avoiding Hypothermia In The Mountains - Part Two
By Gregg Beisly
Winter is upon us and many of us will be out in the hills having fun and the occasional epic that will be fun in the retelling. Before you get on the snow and ice, make sure you are schooled up on keeping yourself safe.
In this three- part series we are looking at how to keep warm, understand hypothermia and manage an emergency situation in cold conditions.
Part 2 Avoiding and Treating Hypothermia
Key Points:
Avoid hypothermia:
‘No knowledge of hypothermia’ is one of the major conditions that leads to hypothermia. Understand how hypothermia occurs and its symptoms.
Prepare:
Fitness helps you sustain activity, which keeps you warm.
Take equipment and wear clothes that you know work for the conditions expected. Test it before really needing to rely on it.
Take enough food and drink to keep hydrated and energy levels high.
Stay dry:
Wet skin and clothing increases heat loss massively. Add wind and you have (typical for New Zealand) conditions with potential for hypothermia.
Stages of Hypothermia:
- Mild - Core body temp below 35°C.
- Moderate - Core temp below 32°C.
- Severe - Core temp below 28°C.
Symptoms
General: Watch for the ‘umbles’: Stumbles, mumbles, fumbles and grumbles.
Mild: Shivering, alert but difficulty with physical tasks.
Moderate: May be shivering, great difficulty with physical and cognitive tasks.
Severe: Unconscious.
Treatment
All: Get patient into shelter, dry clothes and rewarm. Insulate from ground/snow.
Mild: Give high calorie food and drink, patient sits/lies down for 30 mins.
Moderate: Keep horizontal and well wrapped with layers. No drink/food.
Severe: As for Moderate. Handle carefully.
What is Hypothermia
Hypothermia is defined as ‘a decrease in the core body temperature to a level at which normal muscular and cerebral functions are impaired.’
In Part 1 we discussed how to stay warm in cold conditions and how we produce and retain heat. Heat is produced in cells optimally at 37°C. At lower temperatures, this heat output drops. Muscles also perform poorly at lower temperatures, meaning activity is reduced and less heat generated from muscle use.

When you lose more heat than you produce in cold conditions, your body reacts to preserve heat in the most important organs. In order to maintain core body temperature, vascular constriction in the skin and extremities lessens heat loss to the environment by restricting blood flow. Vasoconstriction can decrease cutaneous blood flow from the normal 300-500ml per minute to a miserly 30ml per minute at the minimum end. Cold hands and feet are not too much of a problem, but if you are still losing heat then blood is restricted as much as is needed to protect the core, affecting major muscle groups in the arms and legs, physical activity becomes more difficult and heat generated from muscle activity lessens. Blood will also be restricted to the brain as cooling continues, causing cognitive symptoms—difficulty talking, reduced ability to reason and lack of coordination.

If blood has been restricted to the extremities for some time, what is there will be cold and high in toxins. If the extremities have heat applied to them the result is vasodilation and a rapid return of this relatively cold, stale blood to the heart, dropping the critical core temperature rather than raising it and putting the heart at risk. This phenomena is called ‘afterdrop’ and is why treating moderate to severe hypothermia patients requires some knowledge. Keeping the patient horizontal, limiting limb movement and heating and rewarming slowly reduces the risk of afterdrop. In mild cases of hypothermia, around 30 minutes of sitting or lying while rewarming is recommended before walking as standing increases blood flow to and from the legs, worsening afterdrop. Alcohol is a vasodilator and to be avoided. Don’t give it to a hypothermia patient. Rubbing limbs is also out (sorry Hollywood movies that show either of these as a treatment option).
Shivering is another response from the body to generate heat. This is an increase of chemical reactions required for rapid muscle activity and can increase surface heat production by 500%. Due to depletion of muscle glucose and the onset of fatigue, visible shivering can usually be sustained for only a few hours.
Symptoms of Hypothermia
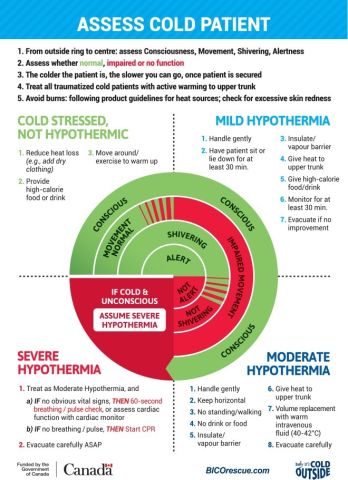
There are a variety of different classifications of how severely hypothermic a person is . Here I will refer to the Wilderness Medical Society clinical staging system. This splits Hypothermia into three groups: Mild, Moderate and Severe. There is also a category before someone is hypothermic—cold stressed. A cold stressed person may be shivering but is alert and can rewarm by their own activity.
The symptoms of mild hypothermia are shivering but otherwise are not functioning normally and are unable to look after themselves.
For moderate hypothermia a person may be shivering or not, depending on if they have depleted all energy reserves. They will be conscious but have great difficulty with simple physical or cognitive tasks. They are unable to care for themselves.
A person with severe hypothermia will be unconscious.
Treatment of Hypothermic Patients
Mild hypothermia:
- Get the patient into shelter. If you do not have emergency shelter and have to move, get insulating and waterproof layers on them.
- When in shelter, remove wet clothing and get them into dry kit with plenty of insulating and waterproof layers.
- Give high calorie food and drink to enable them to keep shivering and avoid dehydration.
- Get them to rest, sitting or lying, for 30 mins (insulate them from the ground!).
- Active warming can be used—warm water in a bottle (or heat pads if available—but not direct on skin) on the chest, back or arm pit.
- Body-to-body rewarming in a sleeping bag can be used, only in mild cases, but is usually no faster at rewarming than shivering alone.
- A warm shower or bath should not be used for initial rewarming (increases afterdrop).
Moderate Hypothermia:
- As for mild hypothermia but handle more gently, and don’t give food or drink.
- The patient should lay down. Insulate them from the ground very well (sleeping pads, packs, ropes…).
- Keep them horizontal.
- Active warming as above with the patient wrapped in layers of insulation—sleeping bag(s) fully done up plus foil layer plus wind/waterproof layer (bivvy bag, bothy bag, plastic pack liners, alpine jackets if not needed…). Insulate the head and around the neck.
- The extremities should not be warmed with a heat source.
Severe Hypothermia:
- As for moderate hypothermia.
- Monitor vital signs (pulse and breathing will probably be difficult to obtain and will be very slow. Check for a pulse for one minute).
- If no vital signs, start CPR.
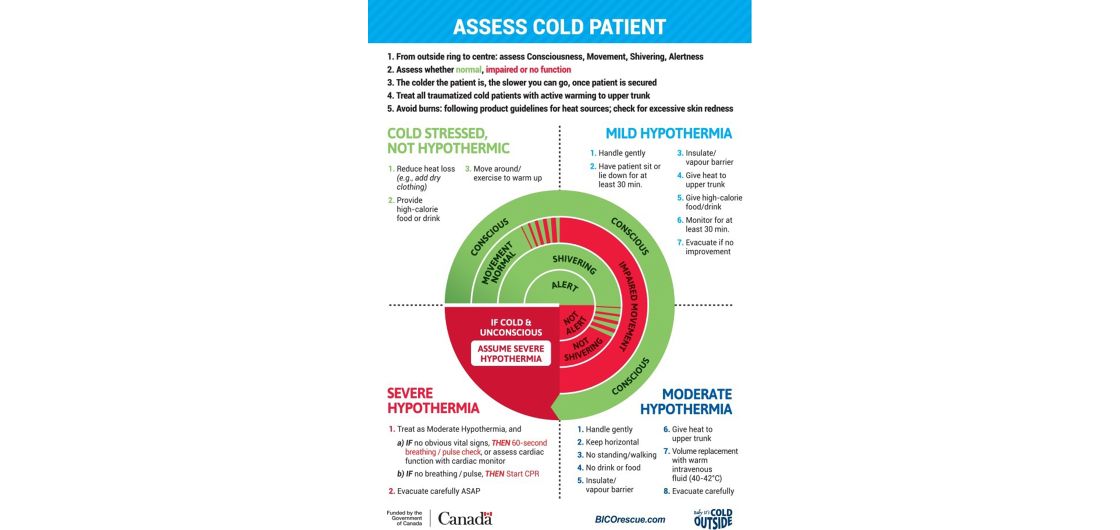
The Wilderness Medical Society has produced the ‘Cold card’ which is free to print and have in your first aid kit as an aid to help you assess and treat hypothermia patients:
Summary
Avoid becoming hypothermic. Prepare adequately for a trip. Take appropriate clothing and emergency kit. Stay dry, block wind, keep well-insulated when not moving, stay hydrated, eat regularly, know the symptoms of hypothermia and look out for others in your group.
In Part Three we will look at how to manage an emergency in cold conditions.
Really great articles these… concise and relevant, thanks
Pagination